A major reason of infection in the respiratory tracts of humans, influenza viruses affect lives of more than 600 million patients annually. In the United States alone, influenza causes as many as 30,000 deaths per annum.
The structure of influenza viruses resembles to that of an encompassed RNA viruses that come from Orthomyxoviridac family. These nucleocapsids are helically symmetric nano-sized particles and composed of a single nucleoprotein containing a multipartite genome of seven to eight segments of single-stranded antisense RNA. Divided on the basis of the varied nucleoprotein antigen constituents, influenza viruses occur in three forms viz. Type A, B and C. Out of them, type A is the most notorious and causes severe damage to human and other host animals. Depending upon whether the surfacing antigen is haemagglutinin (HA) or neuraminidase (NA), the type A influenza virus can be subsequently classified in many subtypes, the most dangerous out of the sixteen HA and nine NA being H1N1 and H3N2.
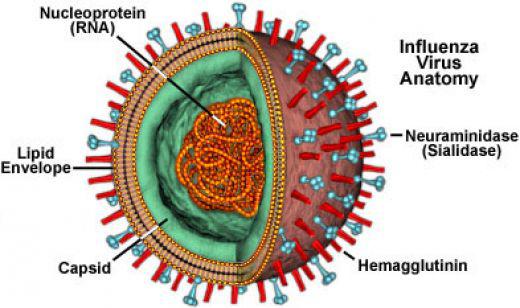
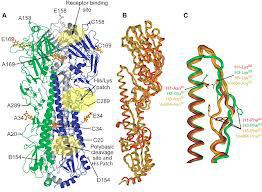
A schematic diagram of H3N2 virus
In an absence of an effective and universally accepted influenza treatment, H1N1 influenza continues to affect the health of many victims in recent years. The government and administrating authorities have shifted their urgent concerns to eradicate or at least cure this disease. In line, the medical fraternity and research agencies have taken this as a challenging task to diagnose and effectively cure the disease right from the stage where symptoms show up in the patients.
The existing guidelines that govern the common diagnosis recommend that patients suffering from influenza-like illnesses during pandemic or epidemic should receive antipyretic treatment with regular administration of ibuprofen or paracetamol. Despite the lack of sufficient scientific evidence supporting its high-utility, medical experts opine that this system of treatment helps the patient with little harm or side-effects.
We will like to attempt a brief inspection on the role of fever in determining whether antipyretic treatment is beneficial in curing influenza or poses the threat to the patient. Monitoring the risks that determine the progress of diagnosis, we can approach towards a more healthy and regulated medical treatment.
Fever and the Defence Mechanism of Host Organism
We can correlate the fever with the phylogenetically antique host response system that is likely to help in survival. Antipyretic treatment can pose risks in terms of various bacterial, viral and other parasite-like microbial infections in humans and other animals. As an immediate response to the emergent infection due to influenza viruses, fever poses quite many beneficial as well as adverse impacts on the patient’s metabolic system as a whole. The increase in body temperature raises the proactive multiplication of active macrophages and lymphocytes thereby facilitating the cytotoxic T cell activity that in turn activates many other cytokines1, for instance, interferon.
There have been several instances to showcase the scarcity of double-blind placebo-controlled randomized clinical trials on the effect of antipyretic therapy on influenza infection in mammals, more so for humans. Due to the lack of substantial placebo group and distorted randomization of antipyretic treatment, there is little assessment of the effects of antipyretics on the severity or the duration of influenza infection in host animals. Quite opposite, however, can be ascertained from the controlled studies of the larger impact of antipyretics and longevity due to influenza infection in some animals.Risking the mortality in animals, a fixed effect pooled odds ratio of 1.32 is observed as a typical effect of antipyretics especially in the analysis of diclofenac and aspirin.
Lacking the solid evidence, probably because of insufficient case studies and relevant experimentation, we cannot confirm the use of antipyretics in treating influenza infections. Based on the results and implications of randomized controlled trials of antipyretics, we can assert that this should be practised and constantly analyzed to
derive the actionable insights.
Dr. B. Cory Harow is an emergency medicine doctor in Boynton Beach, Florida. He received his medical degree from Stony Brook University School of Medicine and has been in practice for 16 years.